Installation of a permanent pacemaker in Türkiye
A permanent pacemaker is a device that sends small electrical impulses to the heart muscle to maintain an appropriate heart rate or to stimulate the lower chambers of the heart (ventricles). A pacemaker may also be used to treat fainting spells (syncope), congestive heart failure, and hypertrophic cardiomyopathy.
Types of pacemakers
There are several types of pacemakers. Your doctor will decide which type of device you need based on your heart condition.
Your doctor also determines the minimum heart rate for setting the pacemaker. When the heart rate drops below the set rate, the device will generate an impulse that will pass through the heart muscle. This causes the heart muscle to contract, which creates a heartbeat.
heart electrical system
The heart is a pump made up of muscle tissue that is stimulated by electrical currents, which usually follow a specific circuit within the heart.
This natural electrical circuit begins in the sinus or sinoatrial node, a small mass of specialized tissue located in the right atrium (upper chamber) of the heart. The SA node generates an electrical stimulus at a rate of 60 to 100 times per minute (adults) under normal circumstances; This electrical impulse from the sinoatrial node initiates the heartbeat.
The electrical impulse travels from the sinoatrial node through the atria to the atrioventricular (AV) node in the lower part of the right atrium.
From there, the impulse continues along the electrical conduction pathway called the bundle bundle and then through the His-Purkinje system to the ventricles (lower chambers) of the heart. When electrical stimulation occurs, it causes muscles to contract and pump blood to the rest of the body. It is the process of electrical stimulation followed by muscle contraction that makes the heart beat.
A pacemaker may be needed when problems occur with the heart’s electrical conduction system. When the timing of cardiac electrical stimulation of the myocardium and subsequent response to the pumping chambers of the heart are altered.
What is a pacemaker?
From an engineering point of view
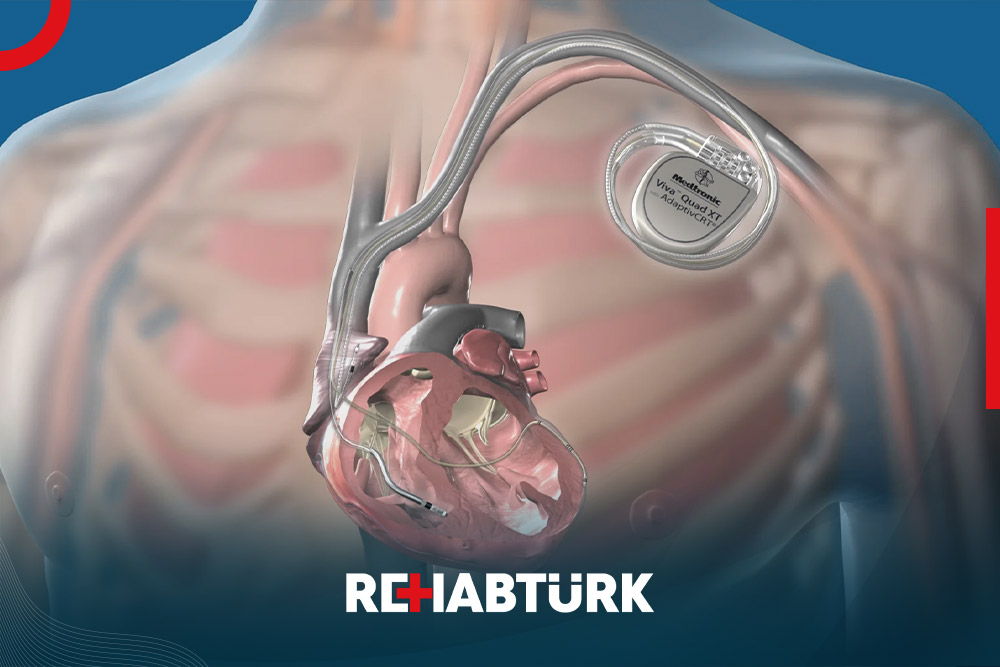
A pacemaker consists of three parts: a pulse generator, one or more wires, and an electrode on each electrode. The pacemaker signals that the heart is beating when the heartbeat is too slow or irregular.
A pulse generator is a small metal case that contains electronic circuitry with a small computer and battery that regulates the impulses sent to the heart.
The lead (or wire) is an insulated wire attached to a pulse generator at one end, with the other end placed inside one of the chambers of the heart. Lead is almost always positioned so that it passes through a large vein in the chest that leads directly to the heart.
The electrode at the end of the lead touches the wall of the heart. Lead conducts electrical impulses to the heart. It also senses the electrical activity of the heart and transmits this information back to the pulse generator. Pacemakers may be placed in the atria (upper chamber), ventricle (lower chamber), or both, depending on the medical condition.
If the heart rate is slower than the programmed limit, an electrical impulse is sent through the lead to the electrode and causes the heart to beat at a faster rate.
The mechanism of action of the pacemaker
When the heart beats faster than the programmed limit, the pacemaker generally monitors the heart rate and will not accelerate. Modern defibrillators are programmed to work only on demand, so they don’t compete with a natural heartbeat. In general, electrical impulses will not be sent to the heart unless the normal heart rate drops below the lower limit set on the device.
A newer type of pacemaker, called a biventricular pacemaker, is used to treat certain types of heart failure . Sometimes in heart failure , the ventricles don’t pump normally.
Ventricular dyssynchrony is a common term used to describe this abnormal pumping pattern. When this happens, the heart pumps less blood. A biventricular pacemaker paces both ventricles at the same time, increasing the amount of blood the heart pumps. This type of treatment is called cardiac resynchronization therapy, or CRT.
After the pacemaker has been inserted, regular appointments will be made to ensure the device is working properly. The doctor uses a special computer, called a programmer, to review the pacemaker’s activity and adjust the settings as needed.
When do you need to implant a pacemaker?
A pacemaker may be inserted in order to stimulate a faster heart rate when the heart is beating too slowly, causing problems that cannot be corrected.
Heart rhythm problems may cause difficulties because the heart is unable to pump enough blood to the body. If the heart rate is too slow, the blood is pumped too slowly. If the heart rate is too fast or too irregular, the chambers of the heart are unable to fill with enough blood to pump out with each beat. When the body does not receive enough blood, symptoms such as fatigue, dizziness, fainting, and/or chest pain may occur.
Some examples of heart rate and rhythm problems for which a pacemaker may be inserted include:
- Bradycardia. This occurs when the sinus node causes the heart to beat too slowly.
- Tachy Brady Syndrome . This is characterized by alternating fast and slow heartbeat.
- heart block This occurs when the electrical signal is delayed or blocked after leaving the sinoatrial node; There are several types of heart blocks.
There may be other reasons for your doctor to recommend insertion of a pacemaker.
What are the risks of implanting a pacemaker?
Possible risks of a pacemaker include, but are not limited to, the following:
- Bleeding from the incision or place where the catheter was inserted
- Damage to the holder at the catheter insertion site
- Injury to the incision or catheter site
- pneumothorax. If the adjacent lung is inadvertently punctured during the procedure, the leaking air becomes trapped in the pleural space (outside the lung but within the chest wall); This can cause breathing difficulties and in extreme cases may cause a collapsed lung.
- If you are pregnant or suspect you may be pregnant, you should notify your healthcare provider.
- In case you are breastfeeding, you should inform your healthcare provider.
Patients who are allergic or sensitive to medications or latex should inform their physician.
For some patients, having to lie flat on the procedure table throughout the procedure may cause some discomfort or pain.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
Before a pacemaker implantation?
Your doctor will explain the procedure to you and offer you the opportunity to ask any questions you may have about the procedure:
- You will be asked to sign a consent form giving you permission to take the test. Read the form carefully and ask questions if something is not clear.
- Tell your doctor if you are allergic or allergic to any medications, iodine, latex, tape, or anesthetic agents (local and general).
- You will need to fast for a certain amount of time before the procedure. Your doctor will tell you how long to fast, usually overnight.
- If you are pregnant or suspect you may be pregnant, you must inform your doctor.
- Tell your doctor about all medications (prescription and over-the-counter), herbal or other supplements, that you are taking.
- Also if you have heart valve disease, you may need to receive an antibiotic before the procedure.
- Tell your doctor if you have a history of bleeding disorders or if you are taking any anticoagulant (blood thinning) medications, aspirin, or other medications that affect blood clotting. It may be necessary for you to stop some of these medicines before the procedure.
- Your doctor may order a blood test before the procedure to determine how long it takes for your blood to clot. Other blood tests may also be done.
- You may receive a sedative before the procedure to help you relax. If you have been given a sedative and there is a possibility that you will be discharged, you will need someone to drive you home. You’ll likely spend at least one night in the hospital after the monitoring is done and to ensure your pacemaker is working properly.
- Depending on your medical condition, your doctor may order another specific preparation.
How is the procedure for implanting a pacemaker?
A pacemaker may be performed on an outpatient basis or as part of your hospital stay. Procedures may vary depending on your condition and your doctor’s practices.
prior to installing the device
- You will be asked to remove any jewelry or other items that may interfere with the procedure.
- Also remove your clothes and you will be given a dress to wear.
- You will be asked to empty your bladder before the procedure.
- If there is excessive hair at the incision site, it may be clipped.
- An intravenous (IV) line will be started in your hand or arm before an injection of medication is given and IV fluids are administered, if needed.
- You will be positioned on your back on the procedure table.
- You will be connected to an electrocardiogram (ECG or EKG) machine that records the heart’s electrical activity and monitors the heart in process using small adhesive electrodes. Vital signs (heart rate, blood pressure, breathing rate, and oxygen level) will be monitored during the procedure.
- Large electrode pads will be placed on the front and back of the chest.
- You will receive a sedative medication into your vein before the procedure to help you relax. However, you will likely remain awake during the procedure.
- The pacemaker insertion site will be cleaned with antiseptic soap.
- Also place sterile towels and sheets around this area.
- A local anesthetic will also be injected into the skin at the insertion site.
During the implantation of a pacemaker
- Once the anesthesia has taken effect, the doctor will make a small incision at the insertion site.
- A casing or insert is inserted into a blood vessel, usually under the collar bone. The sheath is a plastic tube through which the bright lead wire is inserted into the blood vessels and advanced to the heart.
- It will be very important that you remain still during the procedure so that the catheter does not move out of place and prevent damage to the insertion site.
- A lead wire will be inserted through the inserter into the blood vessel. The doctor will push the lead wire through the blood vessels into the heart.
- Once the lead wire is inside the core, it will be tested to verify the correct location and that it is working. One, two, or three lead wires may be inserted, depending on the type of device your doctor has chosen for your condition. Fluoroscopy, (a special type of X-ray that will be shown on a television screen), may be used to help test the location of the sutures.
- The pacemaker generator will be slipped under the skin through the incision (just below the collar bone) after the lead wire is connected to the generator. Generally, the generator will be placed on the non-deployed side. (If you are left-handed, the device will be placed in your upper left chest. If you are left-handed, the device will be placed in your right upper chest.)
- The EKG will be monitored to make sure the pacifier is working properly.
- The skin incision will also be closed with sutures, adhesive tapes, or special glue.
- A sterile bandage or bandage will also be applied.
After a pacemaker implantation?
in the hospital
After the procedure, you may be taken to a recovery room for observation or returned to a hospital room. A nurse will monitor your vital signs.
You should inform the nurse immediately if you feel any chest pain or tightness, or any other pain at the incision site.
After completing the bed rest period, you can get out of bed with assistance. The nurse will help you the first time you get up, and will check your blood pressure while you are lying in bed, sitting and standing. You should move slowly when getting out of bed to avoid any dizziness from the bed rest period.
You will be able to eat or drink once you are fully awake.
The insertion site may be sore or painful. Pain relievers may be given if needed.
Your doctor will visit with you in your room while you recover. Your doctor will give you specific instructions and answer any questions you have.
Once your blood pressure, pulse, and breathing are stable and you are alert, you will be taken to a hospital room or discharged home.
If the procedure was performed on an outpatient basis, you may be allowed to leave after completing the recovery process. However, it is common to spend at least one night in the hospital after implantation of a monitoring pacemaker.
You should arrange to have someone drive you home from the hospital after your procedure.
at home
You should be able to return to your daily routine within a few days. Your doctor will tell you if you will need more time to return to your normal activities. You should not do any lifting or pulling of anything for a few weeks. You may be asked to limit the movement of the arm on the side where the pacemaker is placed, depending on your doctor’s preferences.
You will likely be able to resume your normal diet, unless your doctor directs you differently.
It will be important to keep the insertion site clean and dry. You will be given instructions about bathing and showering.
Your doctor will give you specific instructions about driving.
Ask your doctor when you will be able to return to work. The nature of your occupation, your general health, and your progress will determine how quickly you can return to work.
Tell your doctor to report any of the following:
- Fever and/or chills
- Increased pain, redness, swelling, bleeding, or other drainage from the insertion site
- Chest pain/pressure, nausea and/or vomiting, profuse sweating, dizziness and/or fainting.
- palpitations
Your doctor may give you additional or alternative instructions after the procedure, depending on your particular situation.
How can I book for in Türkiye?

- Free medical support on the phone: You will have a dedicated representative for your health condition who is always ready to answer your questions.
- Free consultation with a specialist doctor: Your medical representative will consult with a number of doctors and hospitals to find the best possible treatments.
- Free travel visa arrangement: We will contact the embassy in your country to assist you in obtaining a visa to visit Türkiye.
- Free itinerary planning: We will create a schedule for your medical trip to Türkiye.
- Free translation of documents and reports: We will translate medical documents and reports into Turkish on your behalf.
- Free support and monitoring: We will monitor the stages of treatment and be by your side every step of the way.
- Free instant translation: We will be with you during the treatment stages to provide translation between you and the medical team.
- Free accommodation and transportation coordination: We will book accommodation for you and your companions in Türkiye, along with transportation services.
Contact REHABTÜRK doctors for more information about the procedure and to evaluate your medical condition.
