Osteomyelitis
Osteomyelitis is a severe condition characterized by inflammation and infection of the bone tissue. It can be triggered by a variety of factors, including:

- Bacteria, such as staphylococcus aureus (staph) and streptococcus bacteria, are frequently responsible for infections. These bacteria have the ability to enter the bone through the bloodstream as a result of an infected wound, surgery, or an infection in the vicinity.
- Fungal infections can occasionally lead to the development of osteomyelitis.
- Injuries to the bone through fractures, open wounds, or surgical procedures have the potential to introduce bacteria or fungi to the bone, which can result in an infection.
Who Gets Osteomyelitis?
Osteomyelitis is a rare condition that affects only 0.02% of the population. It can affect both children and adults, although the impact may vary. Individuals with weakened immune systems due to certain health conditions and behaviors are at a higher risk of developing osteomyelitis.
- Osteomyelitis is often caused by diabetes.
- Sickle cell disease
- HIV or AIDS
- Rheumatoid arthritis
- Intravenous drug use
- Alcoholism
- Long-term use of steroids
- Hemodialysis
- Poor blood supply
- Recent injury
There is a greater likelihood of developing a bone infection when undergoing bone surgeries such as hip and knee replacements.
Symptoms
The signs of osteomyelitis are non-specific and change depending on the person’s age. The primary symptoms consist of:
- Bone pain
- Excessive sweating
- Fever and chills
- General discomfort, uneasiness, or a sense of not feeling well (malaise).
- Local swelling, redness, and warmth
- Open wound that may show pus
- Pain at the site of infection
What are the types of osteomyelitis?
There are two main methods for categorizing osteomyelitis, each providing distinct views on the traits of the infection.
1. Categorization based on where something comes from and how long it lasts.
- Hematogenous Osteomyelitis is the prevailing form, where bacteria enter the bone through the bloodstream from distant sites such as an infected wound, pneumonia, or even a urinary tract infection. This type primarily affects children and young adults, particularly focusing on long bones like the femur or tibia.
- Parallel Osteomyelitis: This variety occurs when the bone becomes contaminated as a result of injury, medical procedures, or nearby infections such as bone ulcers or infections in the joints. It is prevalent among adults and can affect any bone that is susceptible to being exposed externally.
- Osteomyelitis caused by vascular insufficiency arises when the bone’s ability to fight off infection is weakened due to inadequate blood flow, which leaves it susceptible to bacteria. This is especially common in long-lasting conditions such as diabetes and peripheral vascular disease.
2. Classification by Severity and Stage:
- Acute osteomyelitis refers to an infection that develops quickly and progresses rapidly, causing intense pain, fever, and inflammation. It is of utmost importance to identify and treat this condition early on in order to avoid any potential complications.
- Chronic Osteomyelitis is a condition that develops gradually, usually as a result of untreated acute osteomyelitis or underlying issues such as poor blood flow. The symptoms of this type of osteomyelitis may be less severe, but the infection can continue and cause damage to the bone, resulting in deformity and other complications.
- Stage I: Confined to the bone marrow.
- stage II: Shallow, affecting the outer layer of the bone called cortex.
- Phase III: Regional dissemination within the bone.
- Stage IV: Present throughout a significant area of the bone and the tissues surrounding it.
These categorizations aid healthcare practitioners in identifying the most suitable methods of treatment for various forms of osteomyelitis. Treatment plans may consist of antibiotics, surgical intervention, immobilization, and supportive measures, depending on the unique circumstances of each case.
How is osteomyelitis diagnosed?

The doctor taking care of your child will begin by conducting a detailed medical history and physical examination, which may reveal symptoms resembling those mentioned earlier, indicating the presence of osteomyelitis. Additionally, further investigations typically involve carrying out blood tests to examine white blood cells and markers of inflammation, which typically increase during an infection. Furthermore, a blood culture might be performed to identify any organisms in the bloodstream that could be responsible for the infection.
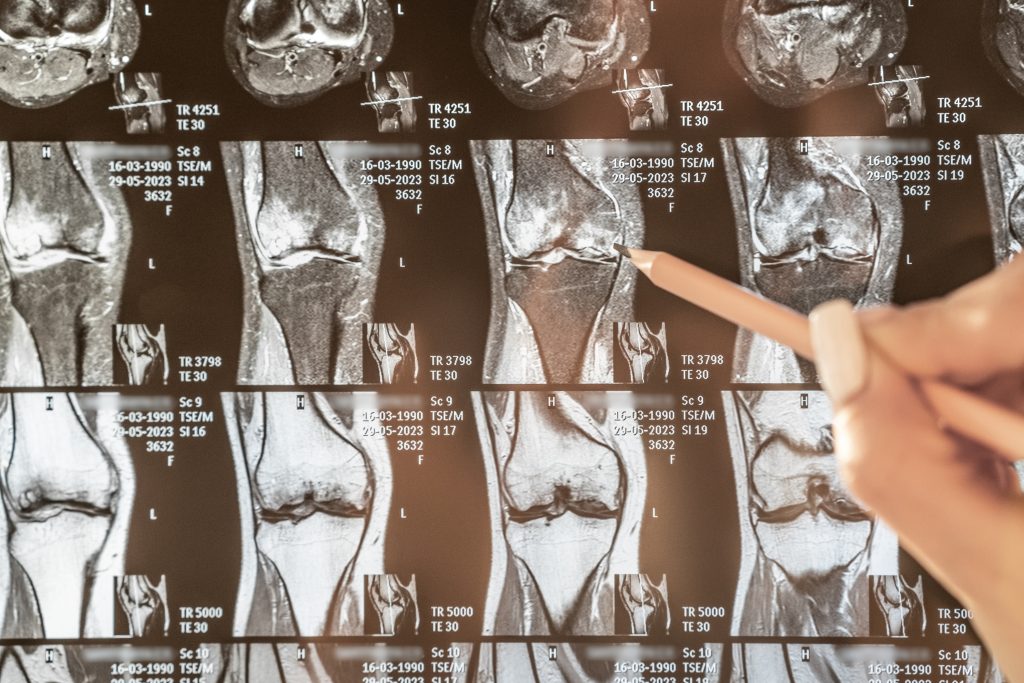
Affected areas are examined using X-rays, but they may not show any abnormalities in the early stages of infection. To determine the cause of bone pain or inflammation, doctors may suggest using magnetic resonance imaging (MRI) or bone scans. In the later stages of osteomyelitis, computed tomography (CT) scans can provide valuable information.
Ultimately, bone aspirations or biopsies play a vital role in identifying osteomyelitis and determining the optimal course of treatment. Typically performed on children, these procedures are commonly carried out in the operating room while the patient is under general anesthesia.
How is osteomyelitis managed or treated?
The management of osteomyelitis consists of two main strategies: combatting the infection and facilitating the healing process of the affected bone. The specific course of treatment will vary based on multiple factors, such as:
- In terms of the infection’s type and severity, it can be classified as either acute or chronic. Additionally, its location, the extent to which it affects the bone, and the presence of any complications are also important factors to consider.
- Medical conditions that are the foundation or basis for other health conditions: examples include diabetes, vascular disease, immune deficiencies, and so on.
- Age and overall health of the patient.
Below is a breakdown of the key elements of the treatment.
1. Antibiotics:
- The main focus of the treatment is to eliminate the bacteria that is causing the infection.
- The specific bacteria identified and the severity of the infection determine the type and length of antibiotic treatment.
- It is common for patients to receive IV antibiotics for a few weeks while in the hospital, and then switch to oral antibiotics for an extended period of time, usually lasting months.
- Regular blood tests and imaging are done to evaluate the effectiveness of treatment.
2. Surgery:
- Often necessary in cases of:
- Extensive damage to the bones accompanied by the presence of deceased tissue (sequestra) necessitating extraction.
- Abscess formation needing drainage.
- Removal of the infected tissue that surrounds the affected area.
- Fixing a broken bone or securing it with surgical implants.
- Whenever feasible, minimally invasive methods are favored in order to minimize harm to the tissues and facilitate the process of recovery.
3. Immobilization:
- Provide relief and support to the impacted region by immobilizing it, either with a cast, splint, or brace.
- Reduce pain and discomfort.
- Prevent fractures in weakened bone.
- Facilitate bone healing.
- The length of time varies depending on the individual situation and how well the healing process is progressing.
4. Supportive care:
- Effectively controlling and alleviating pain through the use of medications plays a vital role in enhancing one’s overall well-being.
- Provision of nutritional assistance might be necessary to guarantee sufficient intake of protein and calories for the purpose of facilitating the healing process.
- Physical therapy can aid in the restoration of physical strength and mobility following a period of immobility.
- Preventing future infections is highly important, and a key step in achieving this is to address underlying medical conditions such as diabetes or vascular disease.
Additional elements to consider:
- Continuous monitoring is crucial throughout and after the treatment to detect any reappearance of infection or potential complications.
- In certain instances, particularly for long-lasting osteomyelitis, it may be necessary to undergo extended treatment with antibiotics.
- It is essential to prevent future infections by practicing good wound hygiene and effectively managing diabetes.
It is important to quickly seek medical help if you suspect osteomyelitis, as this will lead to timely diagnosis and effective treatment, reducing the chance of complications and promoting proper healing.
How can I prevent osteomyelitis?
To avoid infections, it is necessary to clean and treat wounds properly to prevent the entry of bacteria. If you have recently fractured a bone or undergone surgery, or if you have an artificial joint, it is crucial to notify your healthcare professional as soon as any signs of infection arise. However, in numerous cases, it is not possible to prevent osteomyelitis.
Treatment in Türkiye:
The medical staff of surgical teams, doctors, and consultants at REHABTÜRK can provide the best treatment options and free consultations, striving to stay up-to-date on the latest medical technologies and methods.

